Antibiotics are referred to as “wonder drugs” as they are effective against many microbes. However, their offhand use has caused many bacteria to be resistant to them. Antibiotic resistance is responsible for almost 23,000 deaths in the U.S. It is also responsible for an additional medical expense of almost $20 billion.
What is Antibiotic Resistance?
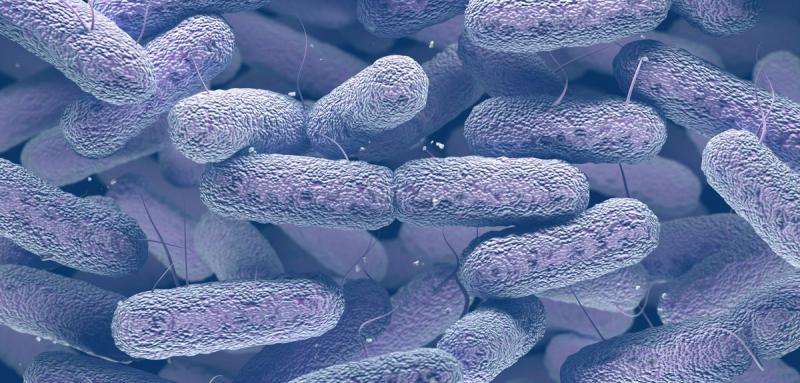
Antibiotics, as mentioned above, fight bacteria. Antibiotic resistance occurs when bacteria continue to multiply even in the presence of an appropriate dose on an antibiotic. Antibiotics create selective pressure and kill the susceptible bacteria. However, a few bacteria can escape this and become resistant to it. Certain bacteria do so by altering a component of the antibiotic, rendering it ineffective. While others export the antibiotic faster before it can do any harm, and some alter their outer structure so that the antibiotic cannot attach to them. All these mechanisms help some bacteria to develop resistance, which can be passed to other bacteria as well.
Below-mentioned are some of the Mechanisms for Antibiotic Resistance:
- Acquired Resistance: A few bacteria can acquire the ability to resist the action of a particular antibiotic to which it was susceptible before. Bacteria can obtain resistance through a genetic mutation, which aids them to survive. They can also acquire this resistance by getting DNA from a bacterium that is already resistant to an antibiotic. For example, Mycobacterium tuberculosis resistance to rifamycin.
- Intrinsic Resistance: In this mechanism, bacteria survive an antibiotic due to intrinsic resistance through evolution by altering their components or structure. Like, an antibiotic that acts by affecting the wall of the bacteria, such as penicillin, cannot be effective against bacteria that do not have a cell wall.
- Genetic Change: Bacterium DNA can alter and change the production of proteins, resulting in different bacterial receptors and components that cause the bacteria to go unrecognized by the antibiotic. An example is Escherichia coli resistance to trimethoprim.
- DNA Transfer: Bacteria can share genetic components, and they can transfer the resistant DNA through horizontal gene transfer (transfer from an organism that is not a parent). Three main steps involved in acquiring external genetic material are transformation, transduction (the process by which a foreign DNA is incorporated into a cell), and conjugation (transfer of genetic material through direct contact). For example, Staphylococcus aureus resistance to methicillin.
Development of Antibiotic Resistance
As antibiotics combat bacteria, it is natural for the bacteria to have the above-mentioned mechanisms to develop resistance against them. However, this increases when antibiotics are used carelessly. As we know, an antibiotic is effective against the majority of bacteria in a colony but those who are genetically mutated can escape their action and become resistant to them. This level of antibiotic resistance is seen to be linked to the degree of antibiotic consumption. Antibiotic resistance also occurs if the complete course of recommended treatment is not taken. Bacteria remain untouched acquiring more strength against that antibiotic. Moreover, resistance is seen to occur in structurally related compounds of the same class.
Are you worried? Well, we all should be. In this war of antibiotic and bacteria, antibiotics are losing the war. If this continues, there will be a time when antibiotics won’t be effective even against common infections like urinary tract infections. Antibiotic resistance treatment is to prevent it. Next time you are prescribed an antibiotic, take its full course and do not share it with anyone.